CPTSD vs. PTSD: Understanding Key Differences & Finding Your Path with Our CPTSD Test
July 27, 2025 | By Beatrice Shaw
Confused about your trauma symptoms? You're not alone. Many find it challenging to distinguish between Complex PTSD (CPTSD) and Post-Traumatic Stress Disorder (PTSD). Questions like "How can I tell if I have CPTSD?" often go unasked. This guide offers clear, compassionate insights into the core differences, helping you understand your unique experience. Gaining this knowledge is an empowering first step toward recognizing your path. For validation and a clearer picture, you can also take our free, confidential CPTSD assessment.
Understanding Post-Traumatic Stress Disorder (PTSD)
PTSD is a well-known mental health condition that can develop after a person experiences or witnesses a terrifying, shocking, or dangerous event. It is a reaction to a specific, often singular, traumatic incident. The mind and body become stuck in a state of high alert, as if the danger is still present, even when it has long passed.
This widely recognized condition presents with a specific set of symptoms that disrupt daily life. The core of PTSD lies in the re-experiencing of a past event that felt life-threatening or posed a significant threat to one's physical or emotional integrity.

What Triggers PTSD Symptoms?
PTSD symptoms are often triggered by reminders of the traumatic event. These triggers can be obvious, like the anniversary of the event, or subtle, such as a particular sound, smell, or even an internal feeling. The brain's alarm system becomes overly sensitive, interpreting safe situations as dangerous. This can lead to intense emotional and physical reactions that feel overwhelming and out of control, a hallmark of this trauma disorder.
Core Symptom Clusters of PTSD
According to clinical guidelines, PTSD is typically defined by four main symptom clusters that cause significant distress:
- Re-experiencing: This includes intrusive memories, flashbacks where you feel like the event is happening again, and nightmares.
- Avoidance: Actively avoiding people, places, conversations, or activities that are reminders of the trauma.
- Negative Alterations in Cognition and Mood: This can involve memory problems, negative beliefs about oneself or the world, feelings of guilt or blame, and a loss of interest in activities you once enjoyed.
- Arousal and Reactivity: This cluster includes being easily startled, feeling tense or "on edge," having difficulty sleeping, and having angry outbursts.
What is Complex PTSD (CPTSD)?
While PTSD often stems from a single event, Complex PTSD (CPTSD) typically develops from exposure to prolonged or repeated trauma, especially when escape is difficult or impossible. This includes experiences like long-term childhood abuse or neglect, domestic violence, being a prisoner of war, or living in a region with ongoing community violence.
CPTSD includes the core symptoms of PTSD, but it also goes further, deeply affecting a person's sense of self and their ability to form relationships. It's the "complex" nature of the trauma—its chronic and interpersonal nature—that leads to these additional, pervasive challenges. Understanding this is a vital part of the healing process, and a cptsd test online can be a helpful first step.
The Role of Chronic and Prolonged Trauma
Unlike a single car accident or natural disaster, the trauma underlying CPTSD is relational and occurs over months or, more often, years. The consistent threat and lack of safety fundamentally shape a person's development, emotional regulation, and worldview. This prolonged trauma erodes one's sense of security and trust, not just in the world, but in themselves and others.
Distinct Symptoms: Disorders of Self-Organization (DSO)
The World Health Organization (WHO), in its ICD-11, officially recognized CPTSD and highlighted three additional categories of symptoms known as Disorders of Self-Organization (DSO). These are what truly set CPTSD apart:
- Problems with Affect Regulation: Intense, overwhelming emotions, including explosive anger, persistent sadness, or suicidal thoughts. It can also manifest as emotional numbness or a feeling of being detached.
- Negative Self-Concept: A deep-seated feeling of being worthless, defeated, or filled with shame and guilt related to the trauma. Survivors often internalize the abuser's voice, leading to a harsh inner critic.
- Difficulties in Relationships: Struggling to feel close to others, maintaining relationships, or feeling a constant sense of distrust and alienation.
CPTSD vs. PTSD: Key Distinctions in Trauma's Impact
While there is overlap, understanding the trauma disorder differences is crucial for validation and finding the right support. The distinction isn't about which is "worse," but about recognizing the unique ways trauma has shaped your life. This clarity empowers self-compassion.
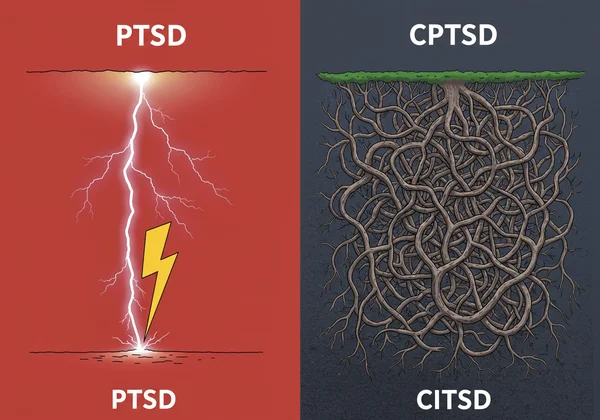
The Nature of the Traumatic Event: Single vs. Ongoing
This is the most fundamental difference.
- PTSD: Often linked to a single event trauma or a short-lived series of events (e.g., combat tour, major accident).
- CPTSD: Linked to chronic trauma that is repetitive and prolonged, often occurring within a relationship where there was an imbalance of power (e.g., parent-child, captor-prisoner).
Emotional Regulation and Dysregulation
While both can involve emotional distress, emotional dysregulation is a core feature of CPTSD.
- PTSD: Emotional reactions are typically tied to triggers reminding the person of the event.
- CPTSD: Emotional dysregulation is more pervasive and can seem to come out of nowhere. It includes chronic difficulty managing intense emotions, leading to outbursts or long periods of depression and shutdown.
Identity, Self-Perception, and Shame
The impact on self-concept is a profound differentiator.
- PTSD: A person's identity is often viewed as "before" and "after" the trauma.
- CPTSD: The trauma is so deeply woven into development that it fundamentally shapes a person's core identity. This often results in a pervasive and toxic distorted self-perception, characterized by deep-seated shame and a belief that they are inherently flawed.
Interpersonal Relationships and Attachment Styles
Difficulties with relationships are central to CPTSD.
- PTSD: A survivor might withdraw from relationships due to fear or lack of interest.
- CPTSD: Survivors often struggle with the very foundation of connection due to betrayals of trust. This can lead to chaotic attachment styles, swinging between desperately seeking closeness and pushing others away out of fear.
Why Understanding Your Trauma Matters for Healing
Why does this distinction matter so much? Because clarity is the first step toward effective healing. Misattributing CPTSD symptoms to a personal failing is a common and painful experience for survivors. Knowing the "why" behind your struggles can change everything.

Validation and Self-Compassion
For many, learning about CPTSD is a life-changing moment of validation. Realizing that your struggles with relationships, emotions, and self-worth are not character flaws but understandable responses to prolonged trauma can lift an enormous burden of shame. This understanding paves the way for self-compassion, a critical ingredient for healing. It allows you to stop blaming yourself and start supporting yourself.
Guiding Your Path to Effective Support and Therapy
Recognizing the specific nature of your trauma helps you seek the right kind of help. While many therapies help with PTSD, healing from CPTSD often requires a more relational and phased approach that specifically addresses the core DSO symptoms. It helps you find therapists who specialize in complex trauma and provides a framework for you to advocate for your needs. Taking a scientifically-backed free cptsd test can provide a starting point for this conversation.
Resumen
Gaining clarity about CPTSD vs. PTSD is more than just an academic exercise; it's an empowering act of self-discovery and kindness. By understanding the key differences in how single-event trauma and chronic trauma impact the mind and body, you can better recognize and validate your own experiences. This knowledge allows you to seek the most suitable support and begin a healing journey grounded in self-compassion rather than self-blame. Remember, you do not have to navigate this journey alone, and understanding is the first step toward finding your path.

Ready to explore your symptoms further and gain personalized insights? Take our free CPTSD test today. It's confidential, based on the WHO ICD-11 guidelines, and designed to help you get a clearer picture of your experience.
Frequently Asked Questions About CPTSD and PTSD Differences
How can I tell if I have CPTSD instead of PTSD?
The key indicator is often the nature of the trauma and the additional symptoms. If your trauma was prolonged or repeated, and you struggle not just with flashbacks but also with deep-seated feelings of worthlessness, intense emotional swings, and chronic relationship difficulties, it may point towards CPTSD. A comprehensive cptsd self-assessment can help you see how your experiences align with these symptoms.
Is CPTSD just borderline personality disorder (BPD)?
No, although they share overlapping symptoms like emotional dysregulation and relationship difficulties, they are distinct. A key difference lies in their origin and core features. CPTSD is rooted in trauma and defined by negative self-concept and disturbances in relationships stemming from that trauma. BPD is characterized by a pervasive fear of abandonment and an unstable sense of self that may exist without a history of complex trauma. A CPTSD vs BPD test can offer initial clarity, but a professional diagnosis is essential.
What is CPTSD commonly confused with besides PTSD?
Besides PTSD and BPD, CPTSD can be misdiagnosed as major depressive disorder, anxiety disorders, ADHD, or even bipolar disorder. This is because symptoms like emotional dysregulation, concentration issues, and persistent low mood are present in all these conditions. Understanding the traumatic context is crucial for accurate differentiation.
Does CPTSD look different in women compared to men?
While the core symptoms are the same, their expression can be influenced by societal gender roles. What does CPTSD look like in a woman? It may more often manifest as "fawn" responses (people-pleasing) or "freeze" responses (dissociation, numbness), which can be internalized and less visible. Men may be socialized to express distress through anger or "fight" responses. However, these are generalizations, and anyone can experience any of the "4 F's" of trauma (Fight, Flight, Freeze, Fawn). Getting personalized insights can help you understand your unique pattern.
Disclaimer: This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. The test on this website is a screening tool, not a diagnostic instrument. Always seek the advice of your mental health professional or other qualified health provider with any questions you may have regarding a medical condition.