我是否患有创伤后应激障碍 (CPTSD)?核心症状与复杂表现
July 21, 2025 | By Beatrice Shaw
您是否经常感到不知所措、不被理解,或者总是隐约觉得有些“不对劲”——但又说不清具体是什么?如果您经历过长期或反复的创伤,您可能正面临着超越典型创伤后应激障碍 (PTSD) 理解的挑战。许多人会问:“ 我如何知道自己是否患有 CPTSD? ” 本指南旨在通过探讨复杂创伤后应激障碍的核心 CPTSD 症状 和复杂表现,为您带来清晰和认同感。
许多人发现,给自己的经历命名是迈向康复的第一步。虽然本文提供信息,但结构化的评估可以提供个性化的见解。为了了解您的经历是否符合,请考虑参加我们的 免费、保密 CPTSD 测试。这是您了解自身情况的简单第一步。

理解基础:什么是 CPTSD 症状?
复杂创伤后应激障碍源于长期或反复的创伤事件,例如持续的童年虐待、家庭暴力或长期的情感忽视。与单一事件创伤不同,这种持续暴露会深刻影响一个人的发展、自我认知以及与他人建立联系的能力。因此,其症状是多层次和多方面的。
要理解 CPTSD,我们首先需要认识到它在 PTSD 基础之上,进一步探究是什么使其“复杂”。这一框架得到了世界卫生组织 ICD-11 的认可,有助于区分该疾病并验证幸存者独特的挣扎。
主要区别: CPTSD 与“普通”PTSD
标准的 PTSD 主要由三个症状群组成:创伤再体验(例如闪回、噩梦)、回避与创伤相关的提醒物,以及持续的威胁感(例如过度警觉)。患有 CPTSD 的个体在经历这些症状的同时,还面临着源于其创伤人际和发展性质的一系列额外挑战。
这一区别至关重要,因为它触及了长期创伤对个人身份和人际关系产生的深刻影响,这是标准 PTSD 诊断未能完全涵盖的。
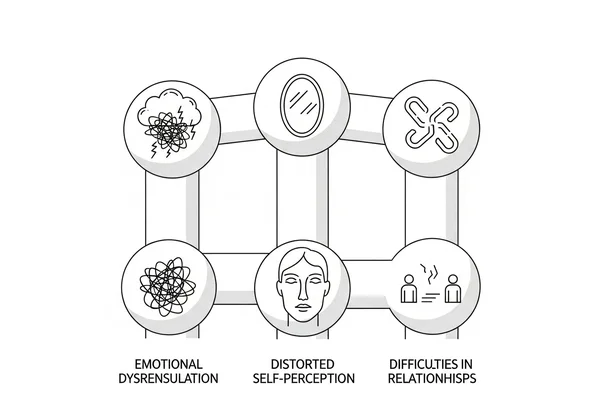
介绍 自我组织方面的紊乱 (DSO)
CPTSD 中的“复杂”一词指的是三个症状类别,称为自我组织方面的紊乱 (DSO)。它们是区分 CPTSD 与 PTSD 的支柱。它们是:
- 情绪失调:在管理情绪方面存在严重且持续的困难。
- 扭曲的自我认知:对自身存在根深蒂固的负面信念。
- 人际关系困难:在建立和维持人际关系方面存在持续的问题。
理解这些 DSO 类别是认识 CPTSD 全貌的关键。
情绪失调 与强烈的情感
CPTSD 最显著的特征之一是难以控制情绪。这不仅仅是感到悲伤或愤怒;而是指情绪感觉压倒性、无法控制,并且常常与当前时刻脱节。幸存者可能会感觉自己一直在情绪的过山车上。
这种强烈的情绪可能会令人困惑和筋疲力尽。CPTSD 自我评估 可以帮助您将这些感受与特定模式对应起来,从而更清晰地了解您所经历的情况。
应对压倒性的 情绪性闪回
与 PTSD 的视觉闪回不同,CPTSD 中的情绪性闪回是指过去强烈的状态在当下涌现。您可能会突然感受到与原始创伤时相同的恐惧、羞耻或绝望感,但没有任何视觉记忆。这些情绪可能由看似微不足道的事件触发,让您感到困惑和失调。
情绪剧烈波动与 管理愤怒/悲伤
CPTSD 的情绪爆发可能感觉毫无征兆,但它通常是对触发因素或累积压力的延迟反应。您可能会经历从麻木到极度愤怒或深切、无法安慰的悲伤的突然转变。这不是性格缺陷;这是神经系统在长期暴露于危险后,难以实现自我调节的一种表现。

扭曲的自我认知: 复杂性 PTSD 的内心世界
长期的创伤,尤其是在童年时期,会向您灌输关于您自己的负面信念。它可能让您产生一种核心信念,认为自己毫无价值、破碎不堪或根本上有缺陷。这些信念成为您看待自己和世界的方式。
这种扭曲的自我认知并非您的过错。它是您所承受创伤的直接结果。承认这些模式是走向自我关怀和治愈的勇敢一步。
深刻的 羞耻、内疚或无价值感
有毒的羞耻感是 CPTSD 的标志。这是一种普遍的感觉,认为你“就是坏”,而不是“做了坏事”。您也可能背负着巨大的内疚感,通常是因为并非您的过错的事情,例如未能阻止虐待或“激怒”施虐者。这些感受可能导致您觉得自己与众不同,与他人隔绝。
持续的 自我批评和自责
您是否有一个严厉的“内心批评者”不断地责骂您?这个声音通常模仿了过去施虐者的言语或态度。它挑剔您的一举一动,将任何不幸归咎于您,并让您相信自己永远不够好。这种无情的自我攻击是一种已经根深蒂固的习得性生存机制。

人际关系与社交连接的挑战
当您的早期人际经历是不安全的,学习信任和建立联系就会变得极其困难。CPTSD 会严重影响您在他人的陪伴下感到安全的能力,从而导致孤立或动荡的人际关系模式。
如果您识别出这些模式,请知悉您并非孤身一人。许多人通过 探索他们的症状 发现,人际关系困难是他们困扰的主要组成部分。
建立和维持稳固关系 的困难
信任他人可能感觉是不可能的。您可能会疏远他人以避免受伤,即使您非常渴望连接。或者,您可能过快建立情感联结,寻求您从未有过的安全感,但最终感到失望,或者当亲密关系感到威胁时将他人推开。
人际关系中的 理想化与贬低 模式
您可能会在将某人捧上神坛,然后在他们不可避免地暴露其人性缺点时又将其贬低之间摇摆不定。这种推拉动态源于对被遗弃的根深蒂固的恐惧和对完美救世主的渴望。这是一个痛苦的循环,可能让您感到长期孤独。
理解 分离:疏离感
分离是一种在无法进行身体逃离时的一种心理上的逃避机制。这是大脑保护您免受压倒性痛苦或恐惧的方式。对于患有 CPTSD 的人来说,它可能成为一种在创伤结束后仍然存在的默认应对机制,让您感觉与自己、身体和世界脱节。
人格解体和现实解体:脱节的体验
人格解体是指感觉自己仿佛在身体之外观看自己,就好像您在看一部电影。现实解体是指周围的世界感觉不真实或模糊不清、扭曲。这些状态,可能是“CPTSD 中的冻结”反应的一部分,会使人感到迷失方向,并可能让人怀疑自己的理智。
记忆缺失 与创伤相关的失忆症
对于长期创伤的幸存者来说,记忆力存在显著的空白,尤其是在创伤期间,这是非常普遍的。您可能难以回忆起童年的大部分时间或特定的事件。这并非记忆力差的迹象;而是分离的强大保护功能。

自我理解与前进之路
接受这些复杂的 CPTSD 症状可能是一次令人不知所措但又极具验证意义的经历。它标志着一个重要的第一步:认识到您的挣扎并非个人缺陷,而是对无法承受情况的自然反应。您寻求清晰的旅程已经开始。
虽然本指南提供了基础,但结构化的评估可以为您独特的经历提供更个性化的见解,帮助您将令人困惑的症状转化为更清晰的图景,并指导您的下一步行动。
准备好了解您的经历是否符合 CPTSD 的情况了吗?您可以 在线参加我们的免费、保密且经过科学验证的 CPTSD 测试 今天以获得个性化的初步评估。该工具基于国际创伤问卷 (ITQ),旨在赋予您宝贵的知识。
免责声明: 请记住,此信息仅用于教育目的,不能替代专业诊断。该测试是一个筛查工具。如果您怀疑自己患有 CPTSD,务必咨询合格的心理健康专业人士。
关于 CPTSD 症状的常见问题
如何在没有正式诊断的情况下判断我是否患有 CPTSD?
您可以开始留意自己是否持续经历我们讨论的症状群:创伤再体验、回避和对当前威胁的感知,以及 DSO 的三个领域(情绪、自我认知和人际关系困难)。基于科学的筛查工具,例如我们的 免费 CPTSD 测验,也可以提供一种结构化的方式来回顾您的症状,并查看它们是否符合 CPTSD 的框架。
患有 CPTSD 的人会面临哪些日常困境?
日常生活可能令人筋疲力尽。常见的困境包括慢性疲劳、注意力不集中、处理工作职责、应对感官超载(如巨大的噪音或明亮的灯光),以及应对感觉令人疲惫或充满威胁的社交场合。当您的神经系统始终处于高度戒备状态时,简单的任务可能会变得异常艰难。
CPTSD 是否等同于边缘性人格障碍 (BPD)?
这是一个常见的混淆点,两者之间存在显著的症状重叠,例如情绪失调和人际关系困难。然而,CPTSD 的核心根植于创伤和负面的自我概念(羞耻、内疚),而 BPD 通常以不稳定的自我感和对被抛弃的恐慌来界定。通过 专业评估 可以帮助明确区分。
CPTSD 发作或触发时感觉如何?
触发因素可以是任何东西——声音、气味、语气——您的潜意识会将其与过去的创伤联系起来。反应或“爆发”通常感觉比当前情况要强烈得多。它可能像一阵突然涌现的愤怒、恐惧或深切的悲伤,完全压倒了您的理性思维。事后,您可能会感到筋疲力尽并充满羞耻,尽管这种反应实际上是您的神经系统试图保护您的方式。